A very important meeting is underway as ACIP, the CDC’s Advisory Committee on Immunization Practices, decides whether the Hepatitis B vaccine — recommended for all newborns since 1991 — should continue to be given in the first days of life or whether that decision should ultimately be left to parents.
As of today, Hepatitis B vaccination is required for public school attendance in nearly every state in the United States. If ACIP votes to end the universal birth-dose recommendation and limit it only to infants born to mothers who test positive for hepatitis B, that long-standing school mandate could be displaced to uncertain ground, since most states base their school requirements on ACIP recommendations.
Hepatitis B is a viral infection primarily transmitted through blood and bodily fluids, most commonly through sexual contact, needle sharing, or exposure during birth. Mothers are routinely tested during pregnancy to determine whether they are hepatitis B positive and at risk of transmitting the virus to their baby. And with only about 0.5% of births involving a mother who tests positive, it continues to raise questions about why the vaccine is recommended for every child on the first day of life.
Also, because newborns don’t engage in sexual activity or needle sharing, the universal vaccination recommendation has puzzled many parents for decades, who wonder why a sexually transmitted or bloodborne illness requires immunization at birth.
Many questions about the safety of the hepatitis B vaccine have been raised by figures such as Robert Kennedy Jr., Dr. Sherri Tenpenny, Dr. Casey Means, and countless concerned parents.
But one CDC contractor, Dr. Cynthia Nevison, walked into the ACIP meeting and raised another critical question: has universal Hepatitis B vaccination, after 34 long years, even lowered Hepatitis B cases on a population level? Dr. Nevison’s answer to that question might surprise you.
And if not the vaccine, why did Hepatitis B cases plummet after 1991? Dr. Nevison addressed that question, too.
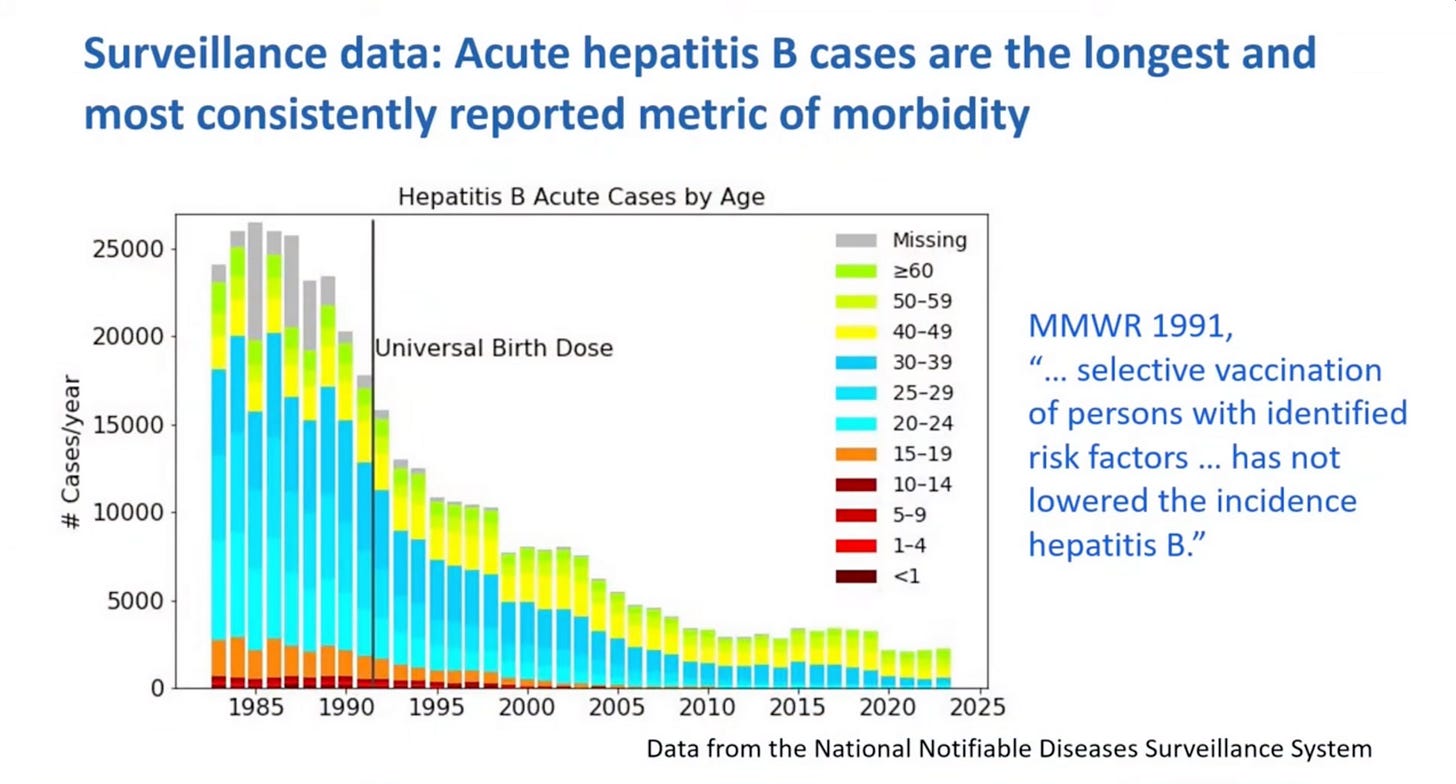
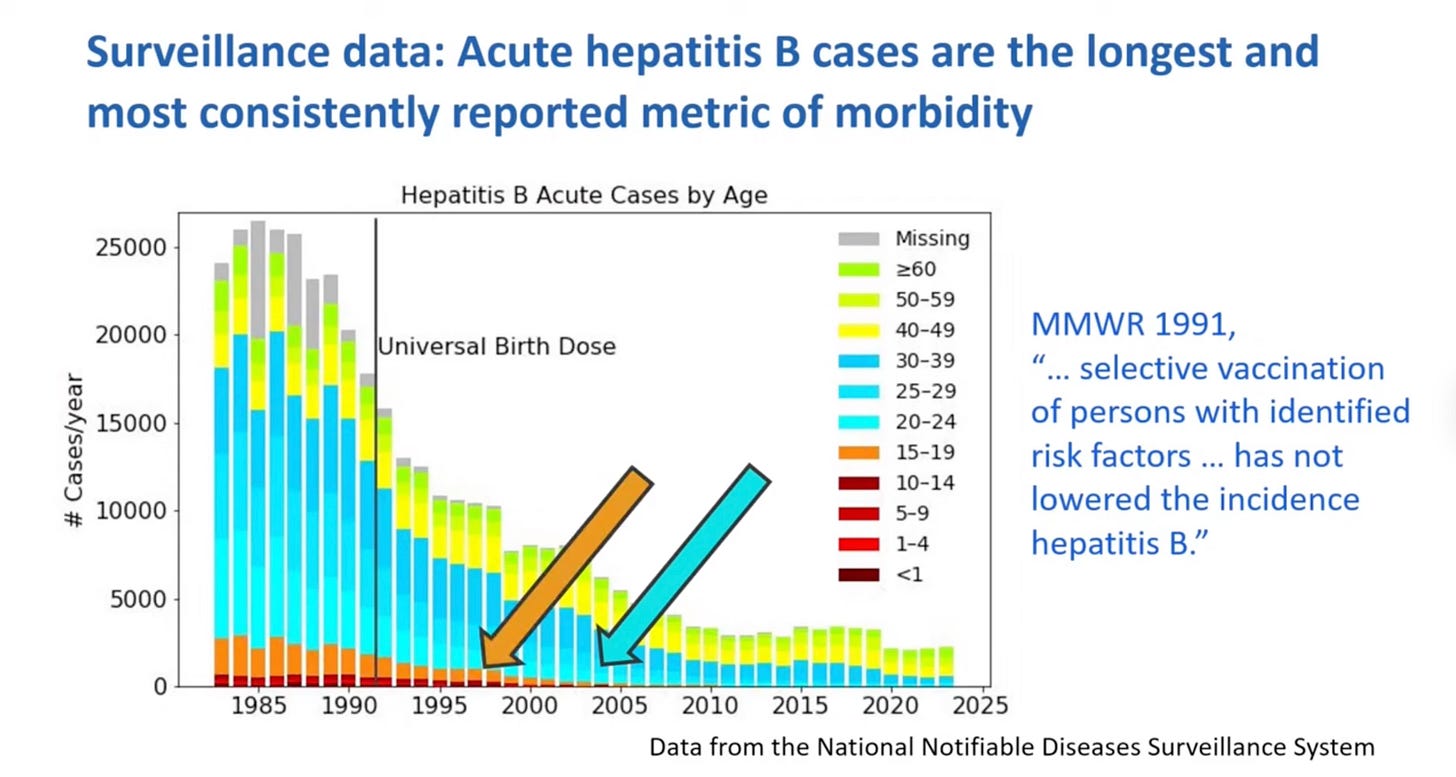
The first slide Dr. Nevison presented showed acute Hepatitis B cases over time. At first glance, it looks like universal vaccination in 1991 is the reason for the downtrend, but if you look closer, you’ll notice that acute Hepatitis B cases were already falling sharply compared to when they peaked in 1985.
Moreover, if you look at the 20–24 (light blue) and 15–19 (orange) age groups, you’ll notice that the rates of acute hepatitis B were falling long before the vaccination could ever be given credit, because the vaccine would not have an impact on 20–24-year-olds until around 2011–2012, or until 2006–2007 for 15–19-year-olds, Dr. Nevison noted.
As such, Dr. Nevison concluded, “universal birth dose contribution to acute [Hepatitis B] case decline is likely very small.”
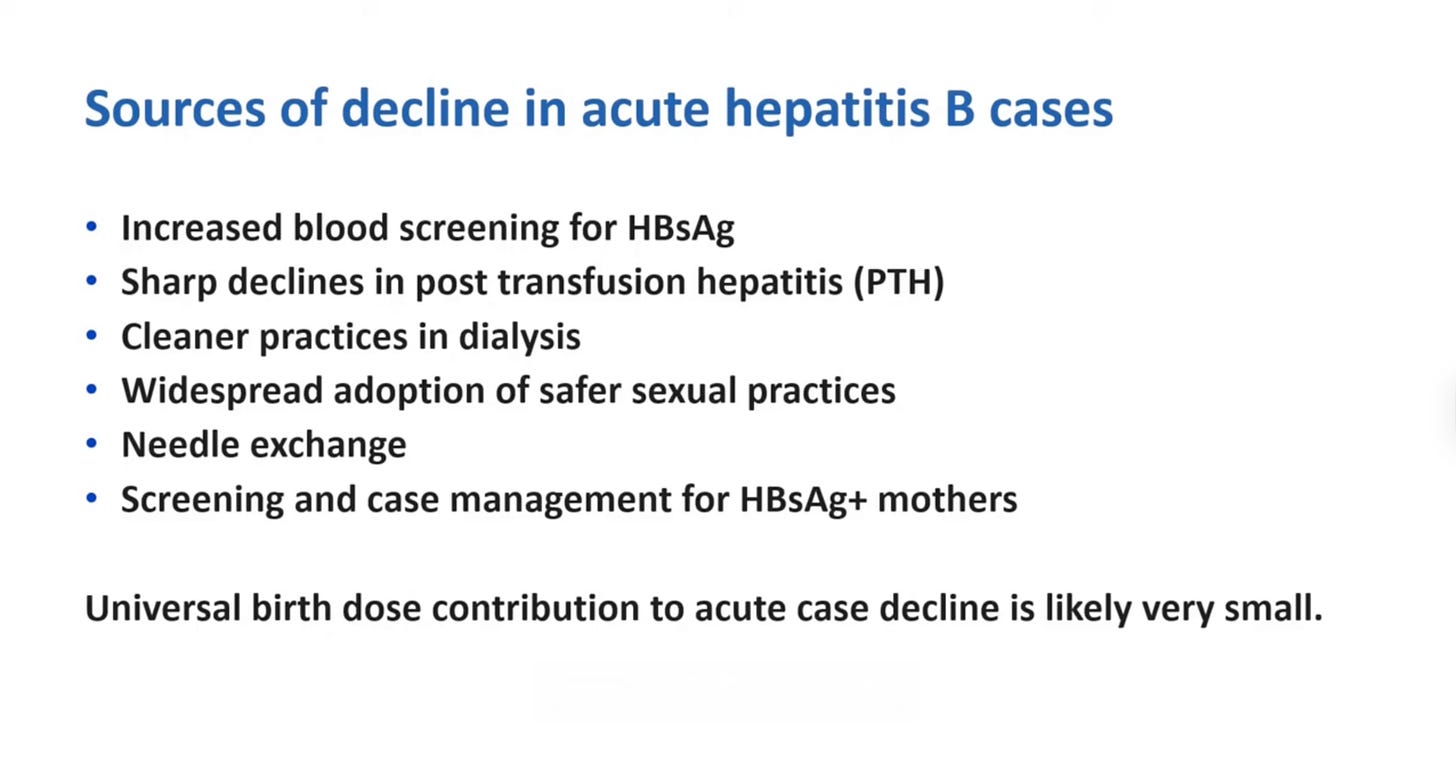
Instead of vaccination, Dr. Nevison gave credit to other factors for the sharp decline in acute Hepatitis B:
• “There was better blood screening for the hepatitis B surface antigen, which led to sharp declines in hepatitis B transmitted through transfusion and also through dialysis.”
• “And then this was the 1980s, with concern about AIDS. So there was widespread adoption of safe sex practices.”
• “And then there were needle-exchange programs, which helped curtail transmission through IV drug use.”
• “And also the 1980s saw the beginning of screening and case management for surface antigen–positive mothers and targeted (not universal) vaccination of their infants.”
“So all these factors helped bring down cases both before the universal birth dose was implemented and after,” she said.
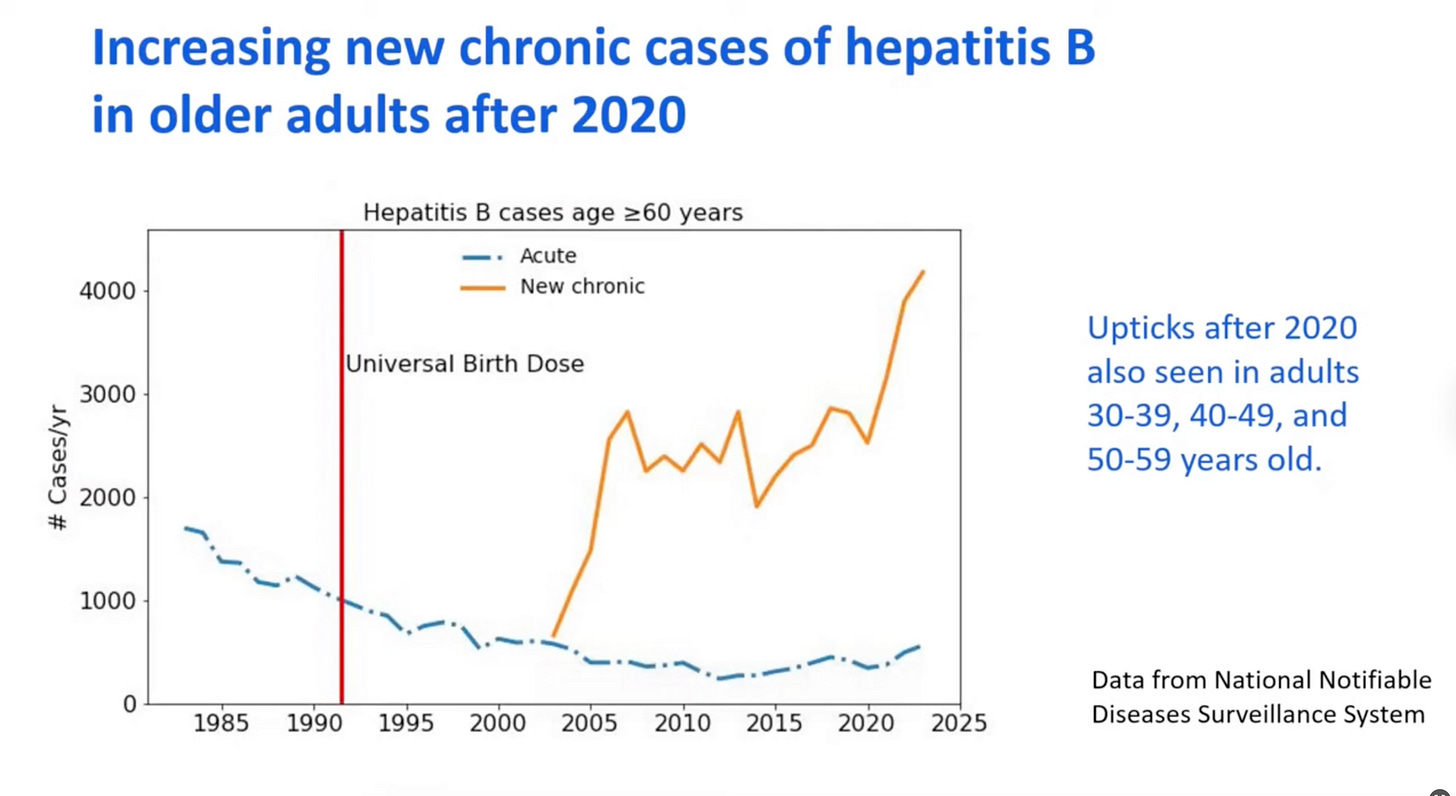
Dr. Nevison showed one last slide on this exact subject, and it was both alarming from a health standpoint and quietly devastating for the universal vaccine program. New chronic cases of hepatitis B have risen sharply in people aged 60 or over since 2020.
Dr. Nevison said, “It’s not clear what’s causing this.” However, “what is clear is the universal birth dose is doing nothing to help these older adults who are experiencing disease now and need help.”
What’s promising is that after 34 long years with little to no debate on this topic, there is now growing pressure to question the legitimacy of hepatitis B shots for newborns on the first day of life.
As we noted, only 0.5% of infants are actually at risk of contracting hepatitis B from the mother, and 88% of mothers are screened. Increasing screening compliance rather than universal vaccination makes far more sense because once you rule out mother-to-baby transmission, the likelihood of a child contracting hepatitis B through sexual contact or needle exposure is virtually zero.
And when you consider that there has never been a true placebo-controlled trial comparing long-term outcomes between vaccinated and unvaccinated children for this shot (or any childhood vaccine, for that matter), it becomes difficult to justify why this vaccination is given universally.
With the leaked FDA memo where Dr. Vinay Prasad wrote that at least 10 children died from the COVID shots, perhaps voting members will come to their senses and recognize that overconfidence in vaccines can have deadly consequences, and that this universal hepatitis B vaccine recommendation makes no sense. We can only hope. We’ll see what happens.
I need your feedback!
Would you like to see more posts like this, where I break down in-depth presentations into a quick and easy read? Was it boring, or do you appreciate the effort? I’d love to hear where you stand.