What Happens When the Body Doesn’t Get Enough Sleep?
One extra or lost hour of sleep makes a bigger difference than most people realize. Dr. Walker explains.
The following information is based on a report originally published by A Midwestern Doctor. Key details have been streamlined and editorialized for clarity and impact. Read the original report here.
“WOW!” Joe Rogan’s brain nearly exploded when Dr. Matthew Walker explained what just a one-hour difference in sleep can do.
When we spring forward for daylight savings time, “we see a subsequent 24% INCREASE in heart attacks.”
But this is the part that blew Rogan’s mind:
“In the fall, in the autumn, when we gain an hour of sleep, there’s a 21% decrease in heart attacks. So it’s bidirectional.”
“Wow!” Rogan said, stunned.
“That’s how fragile and vulnerable your body is to even just the smallest perturbation of sleep,” Dr. Walker explained.
And if losing or gaining just one hour can swing heart attack risk that dramatically, imagine what years of bad sleep are doing to your body.
Sleep deprivation isn’t just making people tired—it’s locking trauma into the nervous system and fueling chronic disease.
When sleep breaks down, emotional injuries don’t heal.
If you don’t get real restorative sleep, your brain can’t process emotional injury, your immune system can’t reset, and your body stays stuck in perpetual stress mode.
That’s not just fatigue—that’s biological harm.
Sleep isn’t a luxury. It’s a physiological necessity for emotional and nervous system healing—and when it’s disrupted, trauma doesn’t fade, it lives in the body.
So why is no one talking about the connection between trauma, sleep, and long-term health?
Trauma isn’t just something that happened to us “in the past.” It can shape our lives every single day.
Trauma is a biological injury that can lodge in the nervous system, quietly reshaping behavior, health, and perception for decades.
It affects us in the past and present and will continue to affect us in the future if not released.
Even small childhood experiences—if left unresolved—can ripple outward into lifelong patterns most people never connect back to the original cause.
Trauma isn’t just the big, obviously traumatic things.
This information comes from the work of medical researcher A Midwestern Doctor. For all the sources and details, read the full report below.
The Profound Consequences of Trauma and Insomnia

While trauma is now widely acknowledged and its deeper impacts are being uncovered, recognition hasn’t translated into effective solutions.
The overwhelming effects of military PTSD and the landmark ACEs (Adverse Childhood Experiences) study made trauma’s long-term health impacts impossible to ignore.
Even the CDC says ACEs are common. Around 61% of adults surveyed said that they experienced at least one form of ACE during childhood.
Unfortunately, the dominant framework still treats trauma as psychological baggage rather than a physiological wound that alters how the body functions.
One of the clearest signals of unresolved trauma is heart disease.
Extreme stress changes vascular tone, inflammation, and autonomic balance—making the heart one of the first organs to fail under prolonged psychological strain.
This isn’t theory. It’s visible in population-level mortality data.
When entire populations are exposed to severe psychosocial stress—war, displacement, cultural destruction—death rates surge.
A Midwestern Doctor addressed the impact of this and putting profit over human life in a 2023 article.
When Industries Value Profit Over Human Life
Most trauma treatments just don’t work.
It’s not because trauma isn’t real, it’s because trauma is misunderstood.
Emotions aren’t abstract thoughts you suppress or reframe until they go away. Trauma is a physical state lodged in the nervous system.
If it stays in the body, healing can’t happen—no matter how much it’s analyzed or talked about.
Western medicine’s materialist model rejects body–mind integration. Most therapies focus on coping instead of resolution. And it turns out that if trauma stays trapped in the body, talking about it without resolving it can actually reinforce the injury.
Trauma doesn’t need management. It needs to be released.
Some people can naturally process trauma. It moves through them and doesn’t get stuck.
Unfortunately, modern society is now encouraging the opposite. Younger generations are being taught to identify with their trauma. They’re holding onto it and literally building their identity around it rather than letting it resolve.
That weakens resilience, lowers stress tolerance, and hardwires emotional triggers.
There’s far more depth on how trauma reshapes the body—and why most treatments miss the mark.
Read the full breakdown by A Midwestern Doctor.
The Profound Consequences of Trauma and Insomnia

Trigger warnings and “safe spaces” were sold as protection. They don’t build strength and resilience. They increase anxiety and reinforce fragility.
Acknowledging real suffering absolutely matters—but institutionalized victimhood has become a tool, not a path to healing.
It’s a recipe for disaster.
Tragically, younger generations are showing widespread autonomic dysregulation.
Minor stressors are triggering panic responses. And constant digital stimulation is keeping their nervous systems locked in fight-or-flight.
Curiously, people with liberal leanings appear to panic more at minor stressors. And media reporting tends to amplify hysteria over events.
Our emotional patterns end up controlling our lives. If we’re stuck in a cycle of victimhood and find our identity in our trauma, where does that lead us?
According to A Midwestern Doctor, emotional health is key in today’s world. And this article on the topic spells it all out:
Emotional Health in the Age of Disconnection
Emotional pain can be addictive. Even more addictive than pleasure.
Trauma often traps people in narratives about blame and injustice, replaying why it happened instead of letting the emotional charge release.
That clenching into emotion locks trauma in place and blocks healing.
When used carefully with experienced guidance, altered states of consciousness—like those induced by psychedelics—can loosen that grip and allow trauma to finally dislodge.
Sleep is one of the most overlooked trauma therapies.
Chronic illness, psychiatric distress, and unresolved trauma almost always disrupt sleep.
Sleep isn’t just about rest. Without restorative sleep, the nervous system can’t reset. The body can’t heal.
The author of Why We Sleep dove deep into the subject with Joe Rogan.
While incredibly common and widely available, most sleep medications don’t actually induce real sleep, the kind we require.
Instead, they sedate the brain while disrupting the cycles our bodies need for repair. Alcohol has a similar effect.
You end up with a person who’s unconscious—but still sleep deprived. That leads to chronic sleep deprivation and even psychiatric instability.
One substance has been able to improve sleep without disrupting its architecture with great success.
But it worked too well and was off-patent. It threatened existing drug markets so it was buried under moral panic.
The result? Inferior and harmful options dominated instead.
Derivatives of the miracle substance, GHB, remain available under strict criteria.
It is heartbreaking to imagine how many lives could have been improved and even saved had GHB not been attacked.
For more information about GHB and the ongoing war against sleep, check out this report from A Midwestern Doctor:
The FDA’s War Against Sleep
It turns out, insomnia is often a drainage problem.
When fluid, pressure, or tension gets trapped in the head and neck, the brain can’t enter deep sleep.
Thankfully, manual decompression and restoring proper flow can dramatically change sleep quality!
Improving zeta potential and relieving sternocleidomastoid tension can be a game changer.
The full article connects it all—trauma, fluid flow, and nervous system repair. And it outlines practical tools most doctors never mention.
Some of them sound almost too simple. All of them point to why fixing sleep often fixes far more than sleep.
The Profound Consequences of Trauma and Insomnia

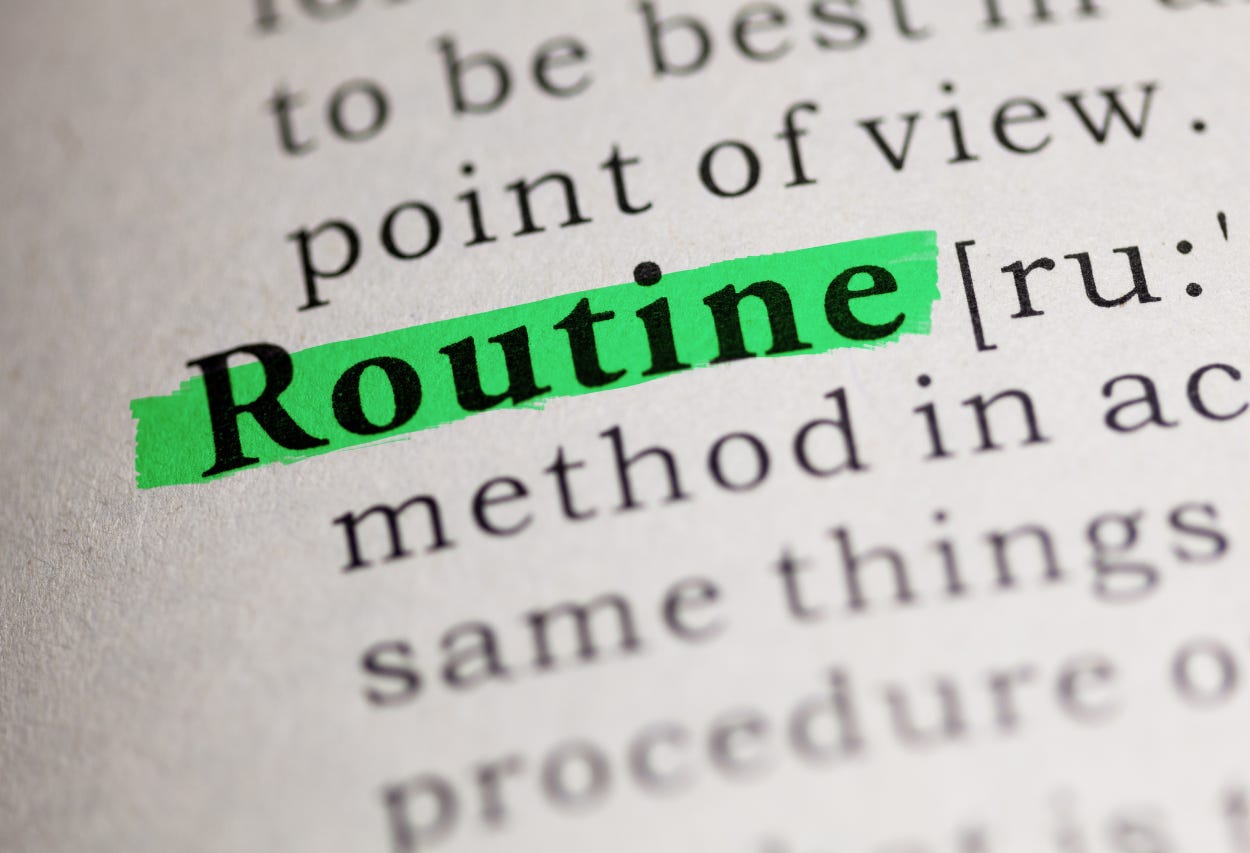
Our modern lifestyle sabotages sleep.
Inconsistent schedules, constant screen exposure, caffeine, and sedentary routines confuse the brain’s circadian signals—keeping the nervous system alert when it should be powering down.
But there are steps we can take to fix this.
Use your bedroom only for sleep
Have consistent sleep/wake times
Have a pre-sleep wind-down period
Avoid excessive computer/sitting time, especially at night
Increase daytime physical activity
Use earplugs to improve sleep quality
Avoid late caffeine intake
Light matters more than most people realize.
Blue light from our devices suppresses melatonin, delays sleep onset, and fragments REM cycles—especially when exposure continues late into the evening.
Try blue light filters, changing the lighting in your home, and using blackout curtains.
There are many simple changes we can all make to improve our sleep, whether or not you’re dealing with trauma.
Hot showers or baths before bed and cooler bedroom environments help your body know it’s time for sleep.
EMFs in your sleeping space can harm sleep. Try turning off your Wi-Fi, putting your phone on airplane mode, and using quality EMF shielding can all help.
REM sleep is where emotional memories lose their charge. REM sleep resolves trauma by removing traumatic emotional attachments to memory.
When REM is disrupted, trauma doesn’t get processed—it gets replayed.
That’s why unresolved trauma often resurfaces as nightmares and chronic hypervigilance.
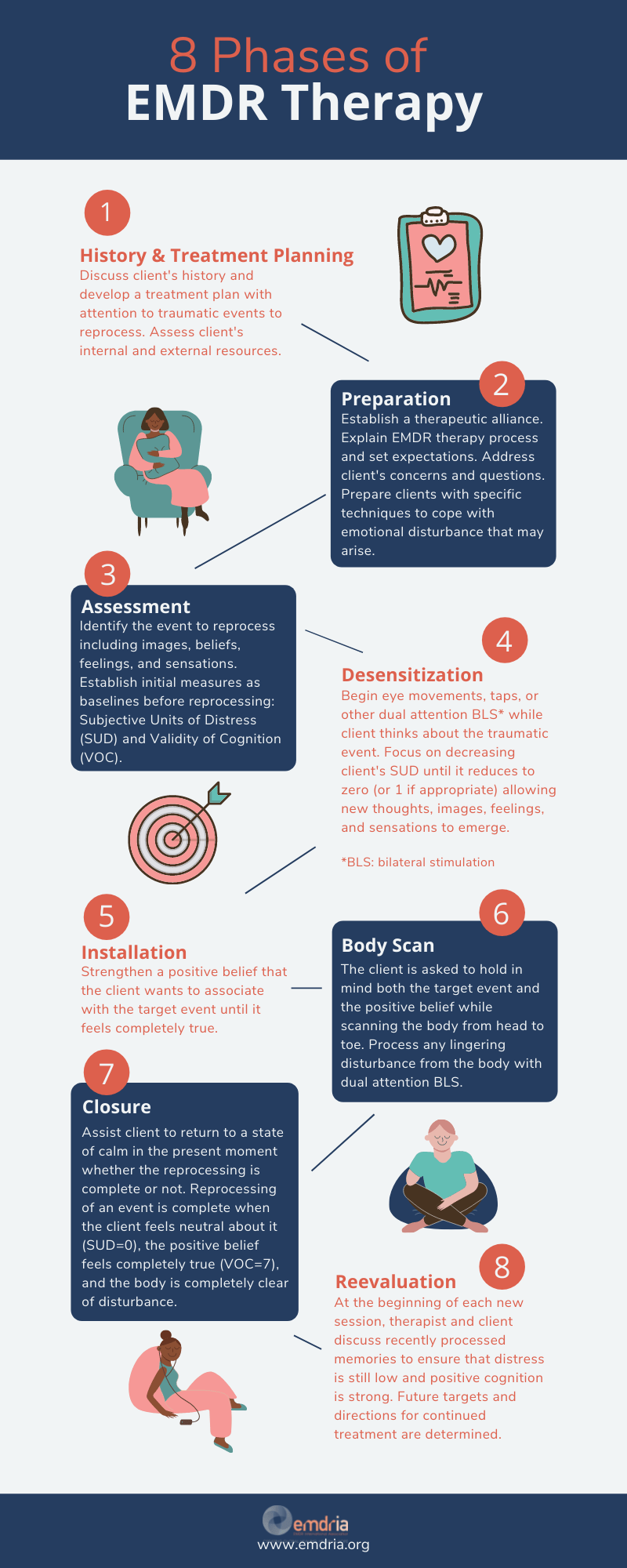
When it comes to treating trauma, EMDR has been very successful. It helps treat traumatic memories by desensitizing emotional responses while recalling the trauma.
EMDR is not perfect, but it works, is covered by insurance, and really should be more widely known.
Years of exploring trauma treatments point to one pattern—approaches that treat trauma as something lodged in the body that must be released work best, even if results aren’t always consistent.
Passive talk-based therapies are easy to sell, but active self-engagement is where real change happens.
Trauma science is still young. It’s evolving fast. Finding the right therapist with the right toolbox is key.
The full article from A Midwestern Doctor goes further and reveals a remarkable resource most people have never heard about.
The Profound Consequences of Trauma and Insomnia

Trauma isn’t destiny.
The body wants to heal—but it needs the right conditions.
Restore sleep. Stop reinforcing injury as identity. Learn how the nervous system releases stress.
Healing isn’t suppression—it’s resolution.
We all deserve to heal, and we all can heal.
Thanks for reading! This information was based on a report originally published by A Midwestern Doctor. Key details were streamlined and editorialized for clarity and impact. Read the original report here.
The Profound Consequences of Trauma and Insomnia

For a deeper dive into what modern medicine has overlooked—or intentionally buried—check out these other eye-opening reports by A Midwestern Doctor:
The Great Cholesterol Scam and The Dangers of Statins
What They Don’t Tell You About C-Sections
What’s The Healthiest Water To Drink?
While you’re at it, give A Midwestern Doctor a follow. No one brings more research, clinical insight, or historical context when it comes to exposing the health myths we’ve all been fed. This is easily one of the most valuable accounts you’ll ever follow.
If you haven’t subscribed to this Substack yet, take a moment to read what some of the most powerful voices in the medical freedom/truth movement have to say:
“The Vigilant Fox has been putting in a lot of work to create a news platform that shares the stories we want to hear about and brings attention to the most important things to know about.”
– A Midwestern Doctor, The Forgotten Side of Medicine
“The Vigilant Fox absolutely is on top of things. We must support our fighters, and the Fox is fighting with truth.”
– Tom Renz, Tom Renz’s Newsletter
“Excellent capture of key video presentations on evolving pandemic science.”
– Peter A. McCullough, MD, MPH, FOCAL POINTS (Courageous Discourse)




















Let’s always stay on Standard Time❣️🕰️
Chamomile tea. 6 bags in a cup. Chamomile essential Do terra oil. And Lavender oil. Also work amazi g.
OR. 4 pellets of Homeopathic Coffea and Chamomile.