An Overlooked Antibiotic Shakes Up the Lyme Disease Debate
In a pair of new studies, one unexpected drug eliminated Lyme bacteria at doses 100x lower than standard antibiotics — without wrecking the gut microbiome.
About 500,000 Americans are diagnosed and treated for Lyme disease every year.
Chances are, you — or someone you know — has dealt with it. Lyme disease often starts as just a tick bite that goes unnoticed, and then it’s accompanied by weeks or months of fatigue, joint pain, or brain fog.
For many people, the most unsettling part comes after treatment. They did what the doctors told them to do. They took antibiotics. And yet, they never fully felt like themselves again.
Lyme disease is common, treatment is standardized, and still a significant number of patients are left with lingering symptoms.
So why do these people still feel so off? The explanation is often murky. Was the infection really gone? Was it autoimmune? Or was it something doctors couldn’t measure — or didn’t fully understand?
That’s why a recent set of studies, as covered by The Epoch Times, caught my attention.
Researchers are closing in on two important advances:
1.) An overlooked antibiotic that clears Lyme infection at dramatically lower doses than the current standard treatment…
2.) And a clearer explanation for why symptoms can persist long after antibiotics are finished.
If you or someone close to you has dealt with Lyme disease, or you’re worried about what happens after a tick bite, this article is worth reading.
Enjoy this free article and explore The Epoch Times’ full catalogue for more daily health insights.
This article originally appeared at The Epoch Times and was republished with permission. Pictures added. Emphasis mine.
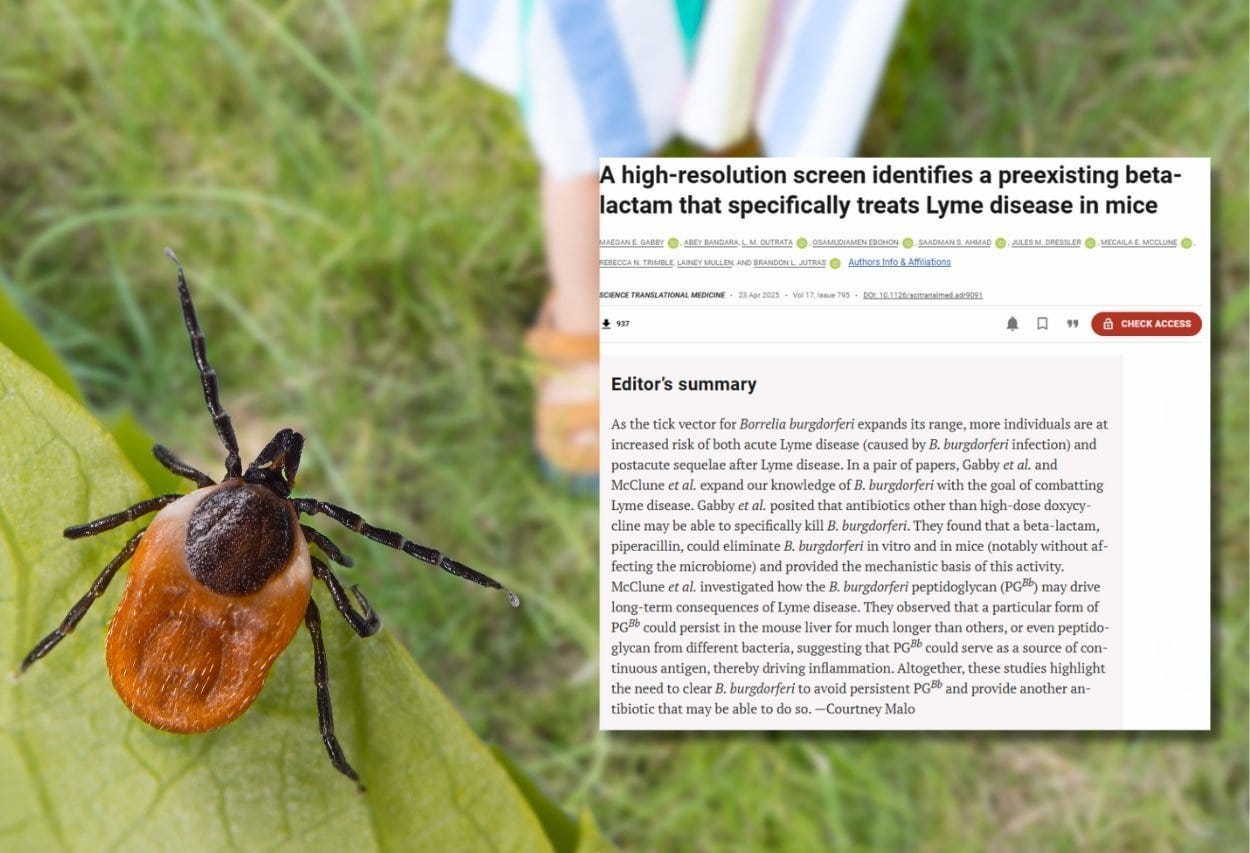
Scientists may be closing in on two major advances in the fight against Lyme disease: an overlooked antibiotic that eliminates the infection at exceptionally low doses and new insights into why symptoms often persist long after treatment.
In a pair of studies published recently in Science Translational Medicine, scientists showed that piperacillin—a Food and Drug Administration-approved antibiotic—cleared Lyme infections in mice at doses up to 100 times lower than those of doxycycline, the current first-line treatment.
Unlike doxycycline, piperacillin targets the Lyme disease bacteria specifically, sparing the gut microbiome from the disruption that typically accompanies doxycycline use.
“What was remarkable to us was how well piperacillin worked at really low doses,” Brandon L. Jutras, a professor in the microbiology-immunology department at Northwestern University Feinberg School of Medicine and lead researcher, told The Epoch Times. “We don’t need to provide it at a concentration that could kill other microbes.”
The team also found that remnants of the Lyme bacteria can remain in the body after being treated with antibiotics, which may explain why some people experience chronic symptoms even after being treated for Lyme infection.
Peptidoglycan—a component of Lyme bacteria’s cell wall—can linger in the body, triggering prolonged immune reactions and helping explain the symptoms of post-treatment Lyme disease (PTLD), where some patients continue to experience symptoms for months or even years after the infection is thought to be cleared.
A More Targeted Approach
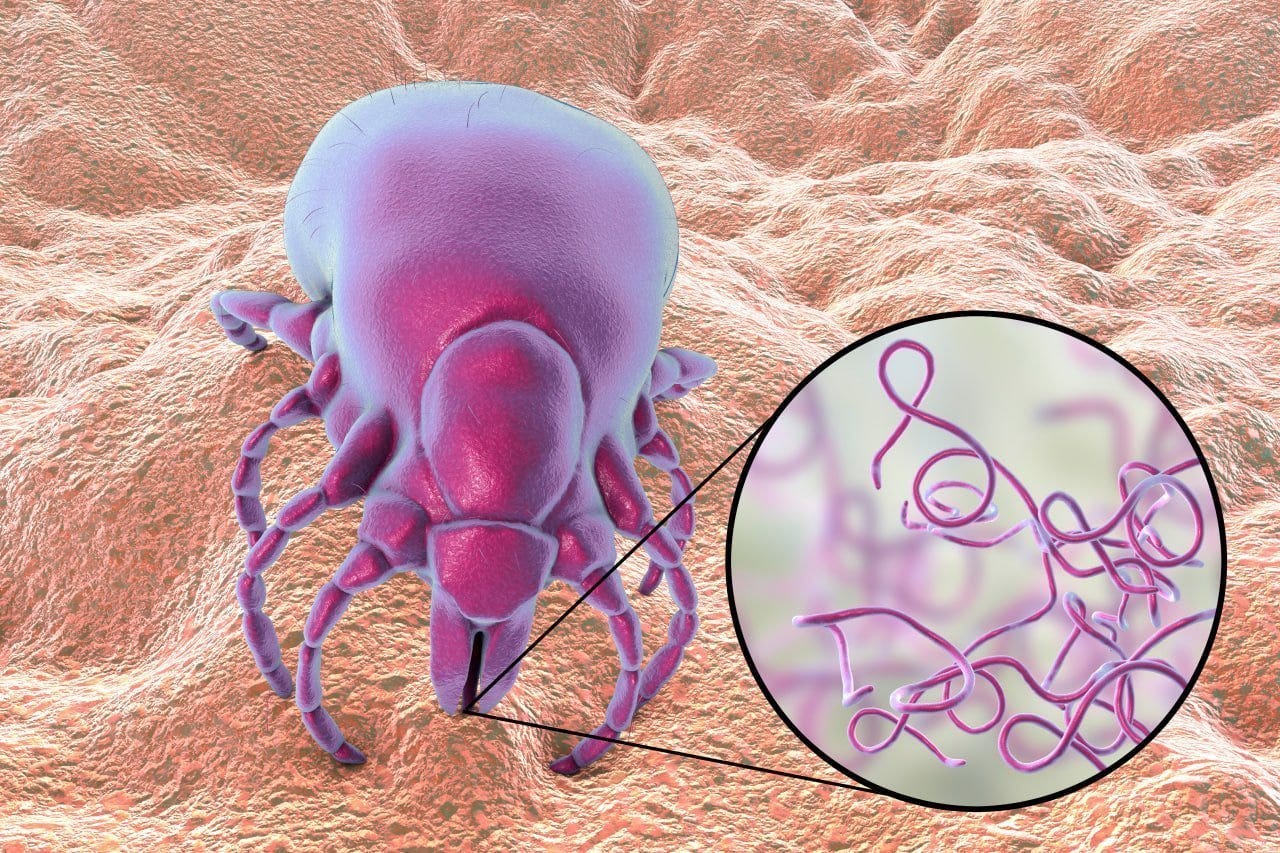
Lyme disease is an infectious illness that is spread to people through the bites of infected black-legged ticks and can lead to neurological and heart complications if untreated.
Piperacillin works by interfering with the unique way Borrelia burgdorferi, the bacterium responsible for Lyme disease, builds its cell walls—a process essential for bacterial survival.
Because of this targeted mechanism, researchers believe piperacillin will spare the gut microbiome, which is often disrupted by broader-spectrum antibiotics like doxycycline. However, whether this more targeted approach could help prevent PTLD wasn’t addressed in the study.
Jutras’s team screened nearly 500 FDA-approved drugs, tracking how each compound affected the bacterium’s ability to build its distinctive cell wall.
“We could literally watch what happened to the cell wall when we added antibiotics,” Jutras said. “Piperacillin disrupted that process in a way that was incredibly specific to Borrelia.”
Currently, piperacillin is used to treat pneumonia and urinary tract infections and is not approved for use against Lyme disease in humans.
Beyond treatment, the researchers also see promise in piperacillin as a potential preventive measure. The idea is that one dose, received right after a tick bite, could stop the infection before it starts.
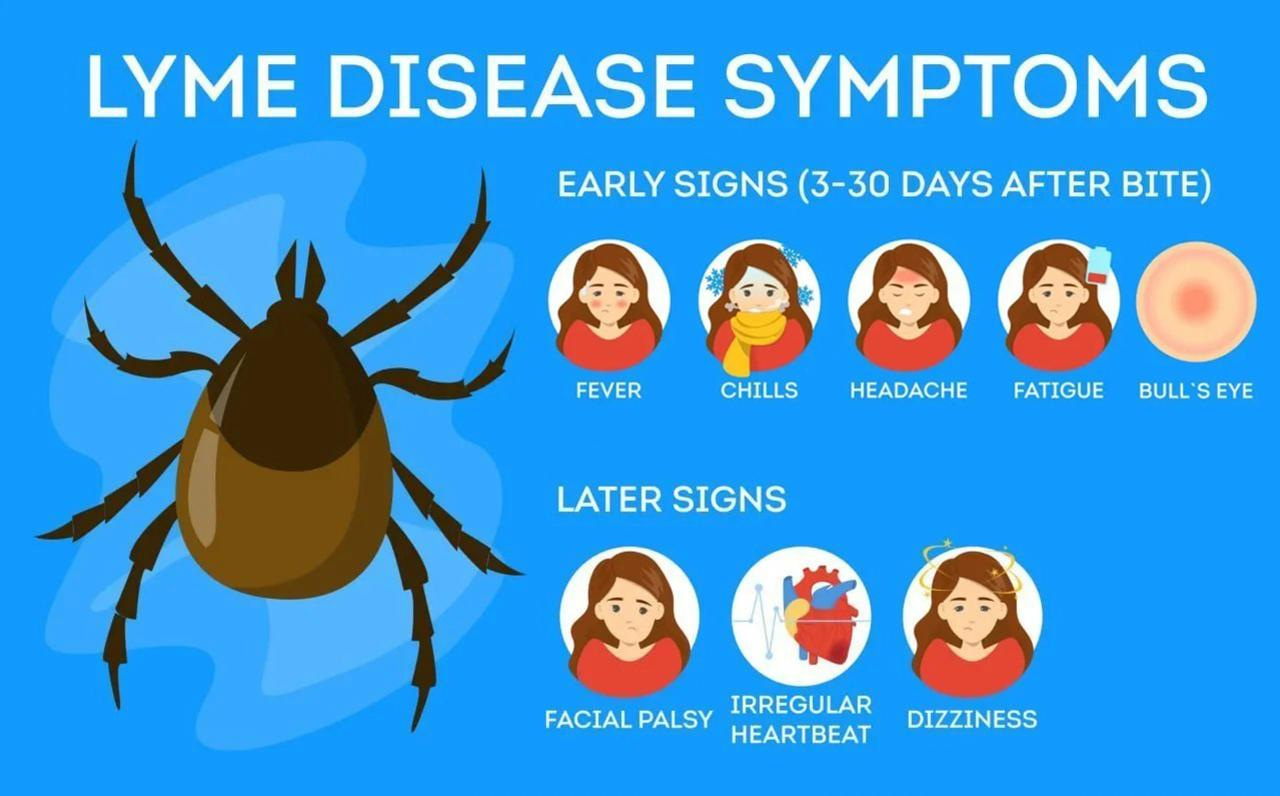
Early diagnosis is challenging since small tick bites may often go unnoticed, early symptoms may not appear for days or weeks, and not all patients develop the telltale bull’s-eye rash.
Diagnostic tests often rely on antibodies that take time to form, resulting in false negatives during early infection.
“You get bit by a tick. You go to your doctor. Right now, they might tell you to wait for symptoms or a positive test result,” Jutras said. “But with piperacillin, the idea is that you could receive a single prophylactic dose. It wouldn’t harm your microbiome, and it might prevent illness altogether.”
Jutras noted that while the findings make piperacillin a promising option, it must first be tested and proven effective in human trials before physicians can prescribe it.
Some experts also caution that any antibiotic—even at low doses—can contribute to antibiotic resistance.
“The question is: does the benefit of potentially preventing Lyme disease outweigh the risk to that person’s microbiome and the collective antibiotic resistance concern that we collectively face?” Dr. Clayton Bell, a physician who specializes in integrative approaches to Lyme disease, told The Epoch Times in an email.
“If piperacillin is proven to be highly effective, then that is a no-brainer in favor of preventing this potentially debilitating medical condition,” he said, adding that piperacillin is only available in intravenous or intramuscular form, so it’s unlikely to be practical for widespread preventive use after a tick bite.
Side effects of doxycycline may include gastrointestinal discomfort, increased sensitivity to sunlight, and potential risks to bone and tooth development in children. It’s also avoided during pregnancy.
Piperacillin, commonly used to treat pneumonia and urinary tract infections in combination with another antibiotic (tazobactam), carries risks of allergic reactions or changes in liver function. However, researchers note that the much lower dose used in this study—and the fact that it was not combined with a second antibiotic—may result in a safer profile.
Why Lyme Symptoms Persist
Lyme disease is now the most common vector-borne disease in the United States, with the Centers for Disease Control and Prevention estimating that approximately 500,000 Americans are diagnosed and treated each year.
Unlike most infections, where the concern is primarily the initial acute phase, a significant worry with Lyme disease is that even after treatment, some people develop chronic symptoms of fatigue, pain, and brain fog that don’t respond to further treatment.
A 2022 study from Harvard University found that 14 percent of those treated for Lyme disease went on to develop PTLD.
There is currently no single approved treatment for PTLD. Management typically focuses on relieving symptoms such as fatigue, joint pain, and brain fog through a combination of supportive care, lifestyle changes, and in some cases, extended or repeated antibiotic courses.
Jutras and his team believe that lingering bacterial debris may trigger an immune response that mimics chronic illness, even when no live bacteria remain. These peptidoglycan fragments were found in the liver and joint fluid of patients with Lyme arthritis, where they continued to provoke an immune response.
Compared with other bacteria, Lyme bacteria’s peptidoglycan is more resistant to breakdown, possibly because of its unique structure—a feature that scientists say is altered by the tick’s biology.
Holistic Approaches for Prevention
To help reduce the risk of persistent symptoms, many doctors who specialize in Lyme treatment take a holistic approach to prevention and recovery.
By lowering the number of lingering pathogens and supporting immune function, these strategies can help manage and even reduce the chances of developing PTLD.
Bell highlighted the importance of identifying co-infections, such as Bartonella, Babesia, Ehrlichia, Anaplasma, or Rocky Mountain spotted fever, as well as addressing mold exposure and mycotoxins. “If co-infections or mold toxins are present and go untreated, the patient will have a much more challenging time recovering from Lyme,” he said.
Herbal remedies such as Cryptolepsis and Japanese knotweed may help reduce bacterial load and strengthen the body’s natural defenses.
Once symptoms indicating an acute infection are gone, these two botanicals may be a superior choice to antibiotics for long-term maintenance therapy after infection, Bell said.
Clean tick bites with soap and water, and remove any attached ticks by using tweezers to pull them upward—without twisting or crushing them.
Early symptoms of Lyme disease, occurring 3 to 30 days after exposure, include:
Bull’s-eye rash (erythema migrans)
Fever, chills, or fatigue
Muscle aches and joint pain
Swollen lymph nodes
Later symptoms, which may occur weeks to months after infection, include:
Severe joint swelling or pain
Drooping on one side of the face (facial palsy)
Numbness or tingling
Irregular heartbeat
Cognitive issues, such as memory loss
Thanks for reading! If you found this valuable, The Epoch Times has a special offer for Vigilant Fox readers:
Unlock their full library of Epoch Health articles — plus everything else on the site — for just $1/week for your first year. That’s 75% off the normal price. Claim it here. Cancel anytime.
More from Epoch Health:
Avoid Taking These 3 Supplements Too Casually as They May Increase Cancer Risk
Popular Artificial Sweetener May Increase Insulin Levels, Research Shows






The problem with antibiotics is they ease the symptoms but don't eradicate the spirochetes.
The attached article explains how Lyme's works. Non-TOA Samento was the only thing that has worked in the past unless there are new things now. I've used it and it works. You have to take it for a full month of dosage. All the spirochetes are killed, but they leave behind eggs. So you take a month off till the eggs hatch, and do another month of samento, which should finish them off. Taking Banderol along with the Samento can enhance the results.
https://www.newswithviews.com/Howenstine/james26.htm
Over 20 years ago, I was exposed over several months to the worst of the toxic molds that I finally found in my condo due to water damage. I was so sick (lungs, brain fog, vision problems) I doubted I’d ever recover. Then I found Dr. Richie Shoemaker in a small town in southern Maryland. It was nearly three hours from my home so I drove and stayed at a B&B. By the way, I could barely stay awake to finish the drive. There, I met the B&B owners whose daughter had been treated by the same doctor for Lyme Disease. They were huge doubters but trusted him because she was pretty sick and he (their family doctor) had never let them down. It turns out we were both prescribed the same drug and she completely recovered, as did I. She had no lasting or residual effects from the Lyme. The drug was Cholestyramine, an old cholesterol reducing medication. In my case, he prescribed that I take it 4 times daily for a month, I think. This med works by getting the biotoxins out of your system and then sending it straight to the gut — no filtering by the liver, which for many people is ineffective for certain toxins. When I returned a month later, having left my condo while they remediated the mold as well as following his orders to a T (that med is nasty tasting!), everything was better. Substantially! No more brain fog, my coughing was almost gone, and the vision problems were much better.
I know it sounds crazy to many reading this, but I hope you’ll look into this further. Antibiotics don’t kill biotoxins, do they? I am guessing the sooner you get the toxins out, the less damage you will have neurologically. Cholestyramine was an accidental discovery by Dr. Shoemaker, but it’s been a lifesaver for many. I should add that his focus has been on mold, but Lyme Disease is a biotoxin too, and I know his protocol works for many (most?) patients he’s treated for Lyme. There’s so much I’ve left unsaid; I hope you’ll check out his website. It says it better than I ever could.
https://www.survivingmold.com/about/ritchie-shoemaker-m-d